- Advanced Trauma Life Support Algorithm
- Atls Guidelines
- Atls Guidelines For Trauma
- Atls Protocol 10th Edition Pdf
Atls 2018.pdf - Free download Ebook, Handbook, Textbook, User Guide PDF files on the internet quickly and easily. ATLS app had not been activated by previous owner so I was able download and sign in on my iPad. Lots of material. Numerous references at the end of chapters for additional study. Bright readable text with pleasing layout.I'm a registered nurse who wishes to pass the ATLS exam and get the certification, its needed for a position I want to.
Abstract
Accidents are the primary cause of death in patients aged 45 years or younger. In many countries, Advanced Trauma Life Support® (ATLS®) is the foundation on which trauma care is based. We will summarize the principles and the radiological aspects of the ATLS®, and we will discuss discrepancies with day to day practice and the radiological literature. Because the ATLS® is neither thorough nor up-to-date concerning several parts of radiology in trauma, it should not be adopted without serious attention to defining the indications and limitations pertaining to diagnostic imaging.
Introduction
In many countries, trauma care is based on Advanced Trauma Life Support® (ATLS®) [1]. Although the ATLS® manual and course are neither evidence based nor up-to-date concerning several parts of radiology in trauma, surgeons use the ATLS® recommendations, if present, routinely to support indications for diagnostic imaging. In addition, surgeons refer to the ATLS® unjustly with indications for imaging that are not supported by the ATLS® at all. Radiologists must be aware of this to intervene appropriately when sub-optimal imaging indications are presented. In this respect, knowing the content and the language of the ATLS can be helpful.
The objective of this review is to familiarize radiologist with the ATLS®. For this purpose, the rationale and indications of diagnostic imaging is assessed where it pertains to the ATLS® protocol. Instances of disagreement with the evidence in the literature and daily practice are highlighted [1].
Purpose of ATLS®
Accidents are the primary cause of death in patients aged 45 years or younger. In The Netherlands, 22 out of 100,000 people die each year because of accidental injury. For every one patient who dies, there are three survivors with serious disabilities [1, 2].
The purpose of adequate trauma care is to decrease this morbidity and mortality, which is expected to be achieved by fast, systematic, and effective assessment and treatment of the injured patient. Contrary to the ATLS guidelines, we think that imaging should play a prominent role in this process.
History of ATLS®
In 1976, an airplane with an orthopedic surgeon, his wife and children crashed in a corn field in Nebraska. The wife died. The surgeon and three of his four children were seriously injured. Although they survived, he considered the standard of care in the local hospital insufficient and decided to develop a system to improve the care for trauma victims, and thus, ATLS® was born.
Since the first ATLS® course in 1978, the concept has matured, has been disseminated around the world and has become the standard of emergency care in trauma patients in 46 countries [1].
The ATLS® concept is also used in the pre-hospital phase of trauma patient care and has been adopted for non-trauma medical emergencies and implemented in resuscitation protocols around the world.
Originally, ATLS® was designed for emergency situations where only one doctor and one nurse are present. Nowadays, ATLS® is also accepted as the standard of care for the first (golden) hour in level-1 trauma centers. The priorities of emergency trauma care according to the ATLS® principles are independent of the number of people caring for the patient.
ATLS® course
The ATLS® course is organized under license of the American College of Surgeons. Before the course, the students peruse the course manual. During a 2-day course, 16 students, mostly residents in surgery and anesthesiology, are trained by eight instructors. These instructors now number more than 100 in the Dutch ATLS® section, mostly surgeons and anesthesiologists but also two radiologists.
During the course, all emergency measures are taught and reviewed. By means of observing, practicing, and repeating the ATLS® concepts, the object of the course is that the students are capable to perform the necessary measures independently with the correct priorities.
The course concludes with a written and practical examination, which has a pass rate of 80–90%.
During the course, attention is also given to the multidisciplinary character of trauma care and the organization and logistics of trauma care in hospitals and surrounding area.
Radiology has a minor part in the course There are only 50 min to teach the systematic evaluation of chest radiographs and another 50 min to teach in cervical spine radiographs, with the objective for the student to be able to identify life-threatening and potentially life-threatening injuries on chest radiographs and identify fractures on the radiographs of the spine. There is no lecture or skill set concerning computed tomography (CT).
Essentials of ATLS®
ATLS® is a method to establish priorities in emergency trauma care. There are three underlying premises. (1) Treat the greatest threat to life first. (2) Indicated treatment must be applied even when a definitive diagnosis is not yet established. (3) A detailed history is not necessary to begin evaluation and treatment.

Therefore, the assessment of a trauma patient is divided in a primary and a secondary survey. In the primary survey, life-threatening injuries are diagnosed and treated simultaneously. All other injuries are evaluated in the secondary survey.
Primary survey
In the primary survey, the mnemonic ABCDE is used to remember the order of assessment with the purpose to treat first that kills first (Table 1). Airway obstruction kills quicker than difficulty of breathing caused by a pneumothorax, and a patient dies faster from bleeding from a splenic laceration then from a subdural hematoma.
Table 1
In the primary survey, the mnemonic ABCDE is used to remember the order of assessment with the purpose to treat first that kills first
| The ABCDE | |
|---|---|
| A | Airway and C-spine stabilization |
| B | Breathing |
| C | Circulation |
| D | Disability |
| E | Environment and Exposure |
Injuries are diagnosed and treated according to the ABCDE sequence. Only when abnormalities belonging to a letter are evaluated and treated as efficacious as possible can one continue with the next letter. In case of deterioration of a patient’s condition during assessment, one should return to ‘A.’ Imaging should not intervene with or postpone treatment.
A: Airway
The airway is the first priority in trauma care. All patients get 100% oxygen through a non-rebreathing mask. The airway is not compromised when the patient talks normally. A hoarse voice or audible breathing is suspicious; facial fractures and soft tissue injury of the neck can compromise the airway, while patients in a coma are not capable of keeping their airway patent. Endotracheal intubation is the most definite way to secure the airway.
In ‘A,’ the cervical spine needs to be immobilized. As long as the cervical spine is not cleared by physical examination, with or without diagnostic imaging, the spine should remain stabilized.
For the evaluation of ‘A,’ no diagnostic imaging is necessary. Imaging of the cervical spine is just an adjunct to the primary survey and not part of the ‘A,’ specifically because, as long as the spine is immobilized, possible spinal injury is stabilized and diagnostic imaging can be postponed. When ‘A’ is secure, one can continue with ‘B.’
B: Breathing
Breathing is the second item to be evaluated in trauma care.
Tension pneumothorax, massive hemothorax, flail thorax accompanied by pulmonary contusion, and an open pneumothorax compromise breathing acutely and can be diagnosed with physical examination alone and should be treated immediately. Most clinical problems in ‘B’ can be treated with relatively simple measures as endotracheal intubation, mechanical ventilation, needle thoracocentesis, or tube thoracostomy. The lack of a definitive diagnosis should never delay an indicated treatment. To evaluate the efficiency of breathing, a pulse oximeter can be applied.
Injuries, like a simple pneumothorax or hemothorax, rib fractures, and pulmonary contusion, are often more difficult to appreciate with physical examination. Because these conditions have less effect on the clinical condition of the patient, they can be identified in the secondary survey.
A chest radiograph is an adjunct to the primary survey and can be helpful in evaluating breathing difficulties and is necessary to evaluate the position of tubes and lines. When ‘B’ is stabilized, one can continue with ‘C.’
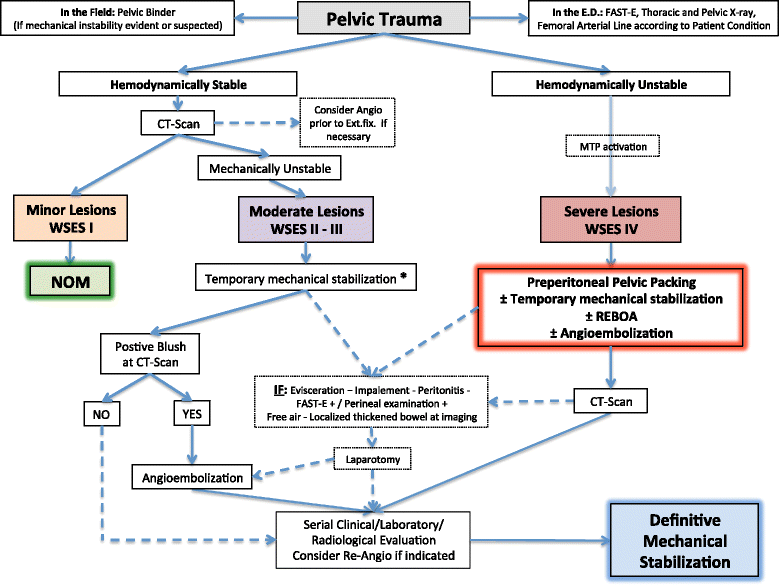
C: Circulation
Circulation is the third priority in the primary survey. Circulatory problems in trauma patients are usually caused by hemorrhage. The first action should be to stop the bleeding. Hemorrhage can be external from extremity and facial injury or not visible from bleeding in chest, abdomen, and pelvis. Instable pelvic fractures can be temporarily stabilized with a pelvic band to decrease blood loss.
Blood pressure and heart rate are measured; two intravenous lines are started, and blood is obtained for laboratory investigation.
In the search for internal blood loss, imaging can be very helpful. Radiological investigations such as a chest radiograph, when not already performed, ultrasound of the abdomen (focussed abdominal sonography in trauma, FAST) and a pelvic X-ray can suggest the localization of the bleeding.
A tension pneumothorax can be the cause of circulatory distress but is usually diagnosed and treated in ‘B.’ When a patient’s condition deteriorates, this diagnosis must be reconsidered. Hemodynamic instability can, infrequently, be caused by pericardial tamponade. Therefore, ultrasonography of the pericardial sac is part of a FAST examination. Other less frequently occurring causes of circulatory problems in trauma patients are myocardial contusion and loss of sympathetic tone caused by cervical and upper thoracic spinal cord injuries.
When it is not possible to stabilize the patient in the trauma suite, other intervention like operation or embolization should be performed. The remainder of the primary survey will be finished thereafter. When ‘C’ is stabilized, one can continue with ‘D.’
D: Disability
Disability should be assessed as the fourth priority in the primary survey, and this includes assessment of the neurological status. The Glasgow coma score (GCS) is used to evaluate the severity of head injury. This score is arrived at by scoring eye opening, best motor response, and best verbal response. Patients who open their eyes spontaneously, obey commands, and are normally oriented score a total of 15 points. The worst score is 3 points. A decreased GCS can be caused by a focal brain injury, such as an epidural hematoma, a subdural hematoma, or a cerebral contusion, and by diffuse brain injuries ranging from a mild contusion to diffuse axonal injury. To prevent secondary injury to the brain, optimal oxygenation and circulation are important. Also, impaired consciousness can be caused or aggravated by hypoxia or hypotension for which ABC stabilization is essential.
If a cranial CT is indicated, it should be done in the secondary survey.
E: Environment and exposure
Environment and exposure represent hypothermia, burns, and possible exposure to chemical and radioactive substances and should be evaluated and treated as the fifth priority in the primary survey.
At the end of the primary survey, before continuing with the secondary survey, the ABCDEs should be re-evaluated and confirmed.
Secondary survey
During the secondary survey, the patient is examined from head to toe, and appropriate additional radiographs of the thoracic and lumbar spine and the extremities are performed when indicated. CT scans, when indicated, are also done in the secondary survey.
If, during the secondary survey, the patient’s condition deteriorates, the primary survey should be repeated beginning with ‘A.’
The rigid spine board should be removed as early as possible because it is a serious risk for decubitus ulcer formation. Removing the hard backboard should not be delayed for the lone purpose of obtaining definitive spine radiographs.
Diagnostic imaging
Radiographs of the chest, pelvis, C-spine, and FAST are adjuncts to the primary survey.
Imaging is considered helpful but should be used judiciously and should not interrupt or delay the resuscitation process. When appropriate, radiography may be postponed until the secondary survey.
CT, contrast studies, and radiographs of the thoracic spine, lumbar spine, and extremities are also adjuncts to the secondary survey.
Imaging is most useful and efficient if consulting with a radiologist becomes routine [, ]. We extrapolate this advice to the trauma setting and endorse consultation with clinicians strongly; however, consulting a radiologist is not mentioned once in the ATLS® manual!
Contrary to (ever-increasing) daily practice, CT plays a minor role in the ATLS®. With the increasing use of CT in the evaluation of trauma patients, radiation exposure should be a major issue in the field of emergency radiology. CT scanners using an automatic exposure control technique can help to reduce radiation dose [, ].
Blunt trauma
Thorax
A chest radiograph must be obtained to document the position of tubes and lines and to evaluate for pneumothorax or hemothorax and mediastinal abnormalities. When not obtained in the primary survey, it should be done in the secondary survey. From the ATLS® manual, it is not clear if a chest radiograph should be performed in every patient [1]. However, this is in accordance with the literature. At present, no clinical decision rule is available concerning the indication for chest radiography in trauma patients.
A CT of the chest is considered an accurate screening method for traumatic aortic injury. If a contrast enhanced helical CT is negative for mediastinal hemorrhage and aortic injury, no additional diagnostic imaging is necessary [1].
If a CT is positive, the ATLS® manual states that the trauma surgeon is in the best position to determine which, if any other, diagnostic imaging is warranted. The possibility to construct multiplanar reconstructions (MPRs), maximum intensity projections (MIPs), volumetric, and virtual angioscopic three-dimensional views from MDCT data, making diagnostic angiography superfluous, is not stated []. The same post-processing tools can be used to differentiate between traumatic aortic injury and normal variants []. Neither consulting with a radiologist nor endovascular treatment of traumatic aortic injury are mentioned in the ATLS® manual.
Although it is recognized that the severity of pulmonary contusions does not correlate very well with the chest radiograph, a CT for the evaluation of pulmonary contusion is not mentioned. The superiority of CT in the detection of pneumothoraces and evaluation of the position of chest tubes is not stated [, ].
Abdomen
FAST is used in hemodynamic abnormal patients as a rapid, non-invasive, bedside, repeatable method to document fluid in the pericardial sac, hepato-renal fossa, spleno-renal fossa, and pelvis or pouch of Douglas. When FAST is available, it replaces diagnostic peritoneal lavage (DPL) []. FAST is a good performing screening tool in evaluating hypotensive trauma patients to differentiate those patients who do need urgent laparotomy from those who do not [].
An abdominal CT is the most sensitive and specific investigation for the diagnosis of visceral and vascular injury; however, according to the ATLS®, an abdominal CT can only be performed in hemodynamically normal patients because a CT is considered time consuming. This is no longer true with the helical CT available today. The rate-limiting step has become the movement of the patient to the CT suite and on and off the CT table [12].
According to the ATLS® manual, an upper GI contrast study is the imaging method of choice in suspected diaphragm rupture. CT is not mentioned as an option. On the contrary, it is stated that CT misses diaphragmatic injuries. Although CT is not 100% sensitive, neither are GI contrast studies. A comparative study is not available. MDCT has the advantage that it is much easier and quicker to perform in trauma patients [1, ]. Although no consensus of opinion exists, coronal, and sagittal multiplanar reconstructions (MPRs) might improve the accuracy of MDCT for the diagnosis of blunt traumatic diaphragm rupture [, ].
A final omission, and contrary to daily practice in many hospitals, is that interventional radiology is not mentioned as an adjunct to non-operative management in patients with abdominal visceral injury [, ].
Pelvis
It is recommended that a pelvic radiograph should be performed when the mechanism of injury or the physical examination indicates the possibility of a pelvic fracture.
Evaluation of the pelvis on an abdominal CT is not mentioned []. Compared to conventional radiography, CT has a higher sensitivity and specificity for the diagnosis of pelvic fractures, and MPRs can be used to delineate the full extend of the fracture [, ].
In a hemodynamically abnormal patient with a pelvic fracture and no indication for intra-abdominal hemorrhage on FAST or DPL, angiography with embolization is advised preceding surgical pelvic fixation.
In patients with an unstable pelvic fracture, inability to void, blood at the meatus, a scrotal hematoma, perineal ecchymoses, or a high-riding prostate, there is a suspicion of a urethral tear, and in these patients, a retrograde urethrogram should be performed before inserting a urinary catheter [1].
To exclude an intraperitoneal or extraperitoneal bladder rupture in patients with hematuria, a conventional or a CT cystogram can be performed [1, ].
Cervical spine
Cervical spine radiographs are not indicated in patients who are awake, alert, sober, neurologically normal, have no neck pain or midline tenderness, can voluntary move their neck from side to side, and flex and extend without pain. In all other patients, a lateral, AP, and open-mouth odontoid view should be obtained. Although it is not mentioned in the ATLS® manual, this seems to be a combination of the Canadian C-spine rules and the Nexus criteria but the criterion ‘painful distracted injury’ has disappeared between the sixth and the seventh edition of the ATLS manual [1, 22–]. Possibly, this was done because the definition of painful distracting injury is difficult, but if omitted, this reduces the sensitivity of the clinical decision rule [].
On the lateral view of the cervical spine film, the base of the skull to the first thoracic vertebra must be assessed. If not all seven cervical vertebrae are visualized, a swimmers view must be obtained and is considered sufficient and safe [1]. Supine oblique views and, contrary to available literature, performing a CT scan of this area is not mentioned [–]. Further, of all suspicious areas and all not adequately visualized areas, an axial CT with 3-mm intervals should be obtained. In the cervical spine section, multidetector CT assessment with coronal and sagittal MPRs is not mentioned at all [1].
Performing a CT of the cervical spine without a preceding conventional radiograph as the screening method of choice is not mentioned. The recent ACR appropriateness criteria suggest otherwise [29].
To detect occult instability in patients without an altered level of consciousness, or those who complain of neck pain, flexion-extension radiographs of the C-spine may be obtained [1]. As flexion-extension radiographs are often non-diagnostic and necessitate movement of the spine that is potentially dangerous, at least, performing a CT first to exclude osseous injury or a magnetic resonance imaging (MRI) for the detection of ligamentous injury should be recommended today [, 29, 30].
MRI is recommended in patients with neurological deficits to detect an epidural hematoma or a traumatic herniated disc. Contrary to the ACR appropriateness criteria, the ATLS states that, when a MRI is not available, CT myelography may be used [1, 29].
Angiography or CT angiography for the evaluation of injury to the carotid or vertebral artery is not mentioned [1].
Head
Again, according to the protocol, a cranial CT should be considered in all head-injured patients with a focal neurologic deficit of which the cause can be localized in the brain, a Glasgow coma scale less than 15, amnesia, loss of consciousness of more than 5 min, or severe headaches. This is insufficient to detect all clinical relevant brain injury. There is no reference to evidence-based clinical decision rules such as the Canadian head CT rule, the New Orleans head CT rule or the CHIP prediction rule [1, –].
Thoracic and lumbar spine
The indications for diagnostic imaging are the same as for the cervical spine. AP and lateral radiographs should be performed with additional CT of suspicious areas [1].
It is not mentioned that the thoracic and lumbar spine can be reliably evaluated on a CT of thorax and abdomen. When a CT of thorax and abdomen has already, or will be, performed, conventional radiography does not have any additional value especially when MPRs of the spine are obtained [].
Penetrating trauma
Advanced Trauma Life Support Algorithm
Chest
Pneumothorax and hemothorax can be diagnosed with a chest radiograph. Even in patients with a normal chest radiograph, a CT is advocated for the evaluation of heart, pericardium, and great vessels in patients with a suspicion of mediastinum transversing injury. For the heart and pericardial sac, a CT can be replaced by ultrasound, and for the major vessels, an angiography can be performed. For the evaluation of oesophageal injury, esophagography using a water-soluble contrast agent and complementary esophagoscopy should be performed. The trachea and bronchial tree can be evaluated by bronchoscopy.
Patients with penetrating injury of the lower chest below the transnipple line anterior and the inferior tip of the scapula posterior are considered to have abdominal trauma as well until proven otherwise [1].
Abdomen
A hemodynamically abnormal patient with a penetrating abdominal wound does not need diagnostic imaging but should undergo laparotomy immediately.
In a hemodynamically normal patient, an upright chest radiograph can document intraperitoneal air and is useful to exclude hemothorax or pneumothorax. An abdominal radiograph (supine, upright, or lateral decubitus) may be useful in hemodynamically normal patients to detect extra-luminal air in the retroperitoneum or free air under the diaphragm.
In all patients with penetrating abdominal injury, an emergency laparotomy is a reasonable option, especially in patients with gunshot wounds. In initially asymptomatic patients with a lower chest wound or injuries to the back or flank, the ATLS® considers double or triple contrast CT, DPL, and serial physical examination less invasive diagnostic options, equivalent to each other [1].
For asymptomatic patients with anterior abdominal stab wounds, DPL, laparoscopy, and serial physical examination are mentioned as diagnostic options. However, although there is a significant body of evidence that this may not be optimal, CT is not mentioned as a diagnostic option in these patients [].
Atls Guidelines
Conclusion
ATLS® is a well-tried systematic approach for the assessment of trauma patients. In multidisciplinary trauma care, it is beneficial and, maybe, even mandatory for effective communication that all members of the trauma team, including the radiologist, speak the same ATLS® language.
Although imaging should not intervene with or postpone treatment, a chest radiograph, pelvic radiograph, and FAST can direct treatment decisions and should be performed in the primary survey when indicated. Imaging of the cervical spine is also an adjunct to the primary survey but can be postponed as long as the spine is immobilized. All other imaging should be done in the secondary survey.
Unfortunately, according to the ATLS®, CT plays a minor role in the evaluation of trauma victims. In the ATLS®, chest CT is only mentioned for the diagnosis of traumatic aortic injury but, in our experience, chest CT is valuable for the evaluation of pulmonary contusions and hemothorax and pneumothorax. Nowadays, abdominal CT is less time consuming than the ATLS® states and can be used to evaluate the extent of the abdominal injury in patients in whom no immediate laparotomy is indicated to evaluate the possibilities for non-operative management with or without endovascular embolization. The indications for head CT according to the ATLS® are insufficient to diagnose all patients with significant head injury. CT of the cervical spine can be used as a primary investigating tool and not only as an adjunct to conventional radiography. When a CT of the chest and abdomen is indicated, the thoracic and lumbar spine, as well as the pelvis, can be evaluated on the axial CT images combined with coronal and sagittal multiplanar reconstructions, and in these cases, conventional radiography of the spine and pelvis do not have any additional diagnostic value.
Because the ATLS® is neither thorough nor up-to-date concerning several parts of radiology in trauma, it should not be adopted without questions to define indications for diagnostic imaging. Consultation between clinicians and radiologists can improve the efficiency and quality of diagnostic imaging in trauma patients.
Abbreviations
| ATLS® | Advanced Trauma Life Support® |
| FAST | focused abdominal sonography in trauma |
| A | airway |
| B | breathing |
| C | circulation |
| D | disability |
| E | environment and exposure |
| CT | computed tomography |
References